WCM-Q researchers investigate key protein that helps explain how obesity leads to type-2 diabetes
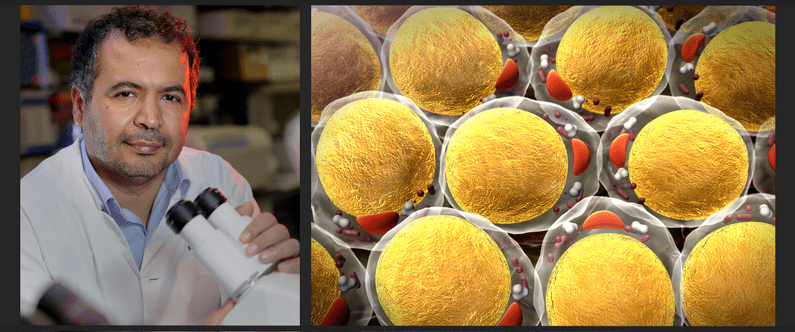 Research led by Dr. Nayef Mazloum of Weill Cornell Medicine-Qatar has shed light on the process by which obesity leads to type-2 diabetes.
Research led by Dr. Nayef Mazloum of Weill Cornell Medicine-Qatar has shed light on the process by which obesity leads to type-2 diabetes.
Researchers at Weill Cornell Medicine-Qatar (WCM-Q) have made new discoveries about the essential role played by a protein called Sirtuin1 in the metabolism of fat, and how depletion of this protein is related to obesity and type-2 diabetes.
The researchers showed that the Sirtuin1 protein – also called SIRT1 – performs a wide variety of important functions, including promoting the metabolism of fat cells, coordinating the generation of healthy new fat cells from stem cells, regulating the function of key metabolic transcription factors and facilitating the transcription of RNA from DNA to set other key metabolic functions in motion.
The research team, led by Dr. Nayef Mazloum, Assistant Professor of Microbiology & Immunology and Assistant Dean for Student Research at WCM-Q, was also able to show that SIRT1 promotes the biogenesis of mitochondria - known as the ‘powerhouses’ of the cell - and facilitates the respiration of fat cells, which is required for fat to be broken down and expelled from the body as carbon dioxide via the lungs. Moreover, SIRT1 promotes the expression of molecules such as leptin, a hormone involved in energy regulation and inhibition of hunger; glutathione s-transferase A3 (GSTA3), a family of enzymes involved in defense against toxic and carcinogenic compounds; and lipocalin 2 (LCN2), which sequesters iron and prevents it being used by bacteria, thus limiting their growth.
The researchers were able to identify these molecular pathways that are dependent on the SIRT1 protein by applying an advanced technique called quantitative proteomics analysis to adipose (fat) cells derived from mouse cells. They were also able to discover that depletion of SIRT1 was associated with dysfunction of the fat cells, leading to increased levels of markers of inflammation and fibrosis of white adipose tissue (fat tissue responsible for energy storage). This is problematic because increased levels of these markers in white adipose tissue are associated with increased risk of obesity-related disorders, including type-2 diabetes. Conversely, supplementing preadipocytes with the NAD+ booster nicotinamide mononucleotide (NMN) during differentiation increased expression levels of leptin, SIRT1, and PGC-1α (responsible for mitochondria biogenesis) and its transcriptional targets, and reduced levels of pro-fibrotic collagens (Col6A1 and Col6A3) in a SIRT1-dependent manner.
Dr. Mazloum said that researchers have known for some time that SIRT1 plays a key role in the human metabolism, but that its precise interactions are still only partly understood. “Our latest research shows us in far greater detail why SIRT1 is such an important protein in human metabolism and metabolic health, playing a key role in many molecular pathways,” he said. “It also underlines that obesity is not just about accumulation of higher levels of stored fat in the body, but that it can also have negative effects on hormone regulation, cellular health, normal fat storage and metabolism, and control of inflammation. We believe that SIRT1 therefore provides us with a very useful target for further research which might ultimately help in the development of new therapies to manage or prevent conditions related to obesity, such as type-2 diabetes.”
The paper, titled SIRT1 promotes lipid metabolism and mitochondrial biogenesis in adipocytes and coordinates adipogenesis by targeting key enzymatic pathways, has been published in Scientific Reports, a leading journal that is part of the Nature portfolio of publications. Other named authors from WCM-Q include Dr. Yasser Majeed, Dr. Najeeb Halabi, Dr. Raphael Courjaret, Dr. Arash Rafii-Tabrizi, Dr. Rudolf Engelke, Dr. Johannes Graumann and Dr. Frank Schmidt. Dr. Aisha Madani, a recent Hamad Bin Khalifa University PhD graduate, also contributed to the project as a member of Dr. Mazloum’s lab. Other institutions that contributed to the study included the College of Health and Life Sciences at Hamad Bin Khalifa University, the Max-Plank Institute for Heart and Lung Research in Germany, the Neurological Disorders Research Center at Qatar Biomedical Research Institute, the Interim Translational Research Institute of Hamad Medical Corporation, Doha, Qatar, CSL Behring, in Bern, Switzerland, and the Biomedical Research Center, at Qatar University.
This research was made possible by National Priorities Research Program (NPRP) Grants NPRP8-059-1-009 and NPRP10-1205-160010 awarded to by the Qatar National Research Fund (QNRF) and Biomedical Research Program (BMRP) funds from WCM-Q, a program funded by Qatar Foundation.
The research can be read in full here.