Introduction
Over the last few years there has been a proliferation in the growth, development and utilization of imaging technology. Radiology has become central to confirming clinical diagnosis, monitoring patient management and in some patients performing minimally invasive treatment. For instance, in the last 2 decades there has been a 12 fold increase in Computed Tomography (CT) examinations in the United Kingdom and a 20 fold increase in overall imaging examination in the USA with an estimated 62 million investigations performed annually 1. This trend is likely to continue as imaging companies strive to deliver safer Xray and CT equipment with lower radiation doses, and Magnetic Resonance imaging becomes cheaper and more freely available to consumers.
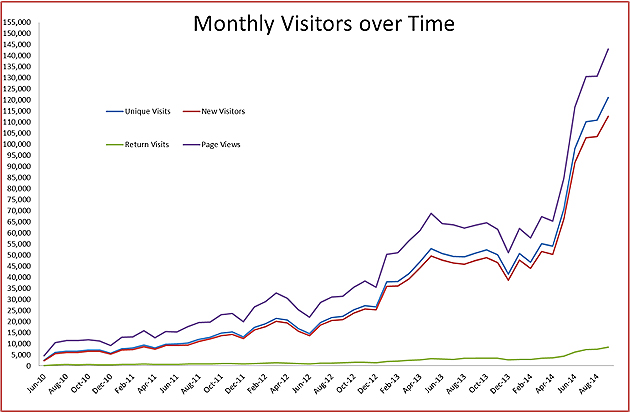
In addition, there has been a significant increase in consumer internet interest in Radiology. One such consumer website, InsideRadiology 2, is showing almost exponential growth in consumer activity and enquiry (see below). Over 2 million hits were recorded on the web site in August 2014 with over 123,000 site visits.
The importance of Radiology in Medical Undergraduate Education has been recognized by the UK Royal College of Radiologists who has established a recommended Radiology teaching curriculum 3. This can be used as the basis for further development and contains a number of suggested topics including:
- Demonstration of Normal Anatomy and basic pathology with imaging
- Radiation Legislation and Patient/Staff Safety
- Nature and choice of imaging investigations
- Patient awareness of the test and experience
- Interaction with Radiology department.
The overall objectives of such a curriculum is to:
- Prepare our young graduates with the required knowledge and skills to choose appropriate examinations, order them, and interpret common pathology,
- Ensure that they appreciate the advantages, disadvantages and safety aspects of each imaging modality,
- Provide them with the confidence and skills to communicate relevant information to Radiology departments, Radiologists, and patients/family under their clinical care.
Current Status of Radiology Education.
There are multiple factors driving academic institutions to continually review, adapt and enhance their undergraduate medical student curriculum programs 4. But despite this continual curriculum review process, there has been little to reflect the increasing importance and demand for Radiology in clinical medicine for both clinicians and patients alike.
A vertically integrated radiology curriculum within a medical school clinical curriculum is uncommon. Only 15% of medical schools in the UK have a formal radiological curriculum in place 1. Of the 34 countries recently surveyed in Europe, radiology teaching started in the first year of medical school in only 26% with most starting to teach Radiology in year 4 5. Rather than following a structured program, Radiology is frequently taught on an ad-hoc basis by clinicians and anatomists with no documented objectives or goals for students. Neither is there any transparent vertical pathway dealing with Radiology topics that can be logically followed through the preclinical and clinical years of training.
In those institutes where formal Radiology programs have been developed and integrated into both preclinical and clinical years, there have been significant improvements in student knowledge. Such curricula at the University of British Columbia (Canada) 6, Al-Baha University (Saudi Arabia) 7, Sydney University (Australia) 4 and more recently Australian National University, Canberra have all shown significant support from both students and clinicians.
The use of imaging in teaching anatomy is well established: 80% of USA medical schools incorporate it in their anatomy courses 8. However, the input of radiology into these courses is only a mere 5% 8 and its absence seems to inadequately prepare students for their future clinical tasks 9. Shober et al. 10 recently surveyed 557 students who undertook a formal Radiology program in their preclinical year. 80% welcomed the introduction of such a program as part of the Anatomy course.
In the UK, clinical Staff specialists interested in undergraduate education indicated that Radiology teaching should be incorporated both in Anatomy and clinical course units. More teaching time needed to be allocated for this to be implemented 11. 58% of newly qualified graduates in New Zealand 12 felt that their Radiology training was inadequate and was only sufficient for them to practice “just safe” medicine.
So as Clinical Educators how are we currently performing? The literature would suggest not very well. New graduates have poor skills in choosing appropriate imaging tests and image interpretation 11. Over 75% of imaging requests submitted to Radiology had inadequate clinical information for making a Radiological diagnosis 13. Graduates have a poor understanding of the safety aspects of imaging and lack the knowledge and expertise to communicate imaging information to their patients. New graduates may harbor negative stereotypes about radiologists 14 which may predispose to antagonism and the concept that Radiologists are “technicians” and not “clinicians”. Most Clinical Radiologists can recount the many hours spent chasing Resident doctors to clarify information on request forms and discussing more appropriate investigations. This has significant impact on Department workflows, and time management.
Future Opportunities
The reason for the deficiency in Radiology teaching is complex. In part it reflects a lack of understanding by clinical educators about the Radiology needs and requirements for new graduates to enable them to interact with their patients and the department. Apart from teaching our students Radiological pathology, we need to provide them with an insight into department logistics, workflows, radiation safety and how these relate to patient care. Most importantly, by the time they graduate, they should be expected to have the skills and knowledge to communicate with Radiologists at a clinical level as well as patients and family at a consumer level. Medical educators should be aware of the significant contribution Radiologists can make at all levels within the Clinical curriculum.
Be that as it may, academic Radiologists have increasing clinical workloads and little time to commit to teaching 14. But where there is a willingness to educate undergraduates, then time must be allocated and incorporated into their Clinical and teaching timetables. If improvements are to be gained in clinical / radiological relationships then Radiologists must take ownership in teaching our students a more holistic approach. The results of this will bring Radiologists back into the clinical domain with improved relationships and better patient health care.
As part of this change in radiology paradigm, Radiologists at the Sidra Medical and Research Center, Qatar, are going to be expected to participate in “point of care” management of patients by relocating traditional Radiologist services outside the physical constrains of the department 15. This same philosophy can be applied even at the undergraduate level: by bringing Radiologists to the classroom, they would be able to interact and engage directly with our students at all levels of the Clinical curriculum. The ease at which multiple images can now be electronically accessed and distributed means that Radiologists have complete freedom to teach anywhere. Bringing mobile imaging modalities eg Ultrasound, to the anatomy classroom can bring a new and exciting level of student participation.
As part of the continuous reassessment and review of clinical curricula, WCMC (New York) recently introduced their new undergraduate program. Radiology teaching has been clearly identified in the Anatomy course and in parts of many of the clinical teaching units. As this transition moves forward, it will be important to look at clearly defined goals and objectives of the radiology curriculum and to map these to outcome measures so we can be sure that our students are going to achieve the knowledge and skills that they require when they graduate.
We are privileged to work and live in an environment in Qatar where patient centered health care and education is financially supported and encouraged. Student numbers are comparatively small so we have the opportunity at WCMC-Q to provide interactive and innovative Radiology teaching. In fact, at recent WCMC-Q orientation for new faculty members, the concept of innovation on our campus was encouraged. WCMC-Q has a great opportunity to lead the way in Radiology education: the provision of such a radiology program will enhance the WCMC curriculum. As mentioned, documentation of clear goals, objectives and outcome measures will assure us that new graduates are well prepared and grounded in Radiology as they transition into clinical practice. Clinical Radiologists should then be able to look forward to working more closely with new WCMC-Q medical graduates with improved understanding, mutual respect and better patient care.
References:
- Bhogal P, Booth TC, Phillips AJ, Golding. Radiology in the undergraduate medical curriculum – Who, how, what and where? Clinical Radiology. 2012;67: 1146-1152.
- InsideRadiology. Statistics provided by Quality and Safety Unit, Royal Australasian and New Zealand College of Radiologists.
- Royal College of Radiologists: Undergraduate Curriculum. http://www.rcr.ac.uk/content.aspx?PageID=2371
- Pascual TNB, Chhem R, Wang SC, Vujnovic S. Undergraduate radiology education in the era of dynamism in medical curriculum: An educational perspective. European Journal of Radiology. 2011;78 (3): 319-325.
- Kourdioukova EV, Valcke M, Derese A, Verstraete KL. Analysis of radiology education in undergraduate medical doctors training in Europe. European Journal of Radiology. 2011.78 (3): 309-318.
- Lee JS, Aldrich JE, Eftekhari, A, Nicolaou S, Muller, NL. Implementation of a New Undergraduate Radiology Curriculum: Experience at the University of British Columbia. Canadian Association of Radiologists Journal. 2007;58 (5): 272-278.
- Al Qahtani F, Abdelaziz A. Integrating radiology vertically into an undergraduate medical education curriculum: a triphasic integration approach. Advances in Medical Education and Practice. 2014;5: 185-189.
- Zafar AM. Radiology: an underutilized resource for undergraduate curricula. Medical Teacher. 2009;31 (3): 314.
- Waterston SW, Stewart IJ. Survey of clinician’s attitudes to the anatomical teaching and knowledge of medical students. Clinical Anatomy. 2005;18: 380-384.
- 10. Schober A, Pieper CC, Schmidt R, Wittkowski W. “Anatomy and Imaging”: 10 years of experience with an interdisciplinary teaching project in preclinical medical education – From elective to a curricular course. Fortshcr Rontgenstr 2014;186: 458-465.
- Miradraee S, Mankad K, McCoubrie P, Roberts T, Kessel D. Radiology curriculum for undergraduate medical studies – A consensus survey. Clinical Radiology 2012;67. 1155-1161.
- Subramaniam R, Hall T, Chou T, Sheehan D. Radiology Knowledge in new medical graduates in New Zealand. The New Zealand Medical Journal. 2005;118: 9-15.
- Sardanelli F, Quarenghi M, Fausto A, Aliprandi A, Cuppone MT. How many medical requests for US, body CT, and musculoskeletal MRI exams in outpatients are inadequate? Radiological Medicine. (Torino). 2005;109 (3): 229-233.
- Gunderman RB. Medical Students are our future. Journal of College of Radiology. 2005;2 (9): 795-797.
- Deepak K. New Qatar hospital will pursue point-of-care radiology. AuntMinnie Middle East.
http://www.auntminnie.com/index.aspx?sec=sea&sub=res&searchsec=all&searchtype=contains&qu=Deepak%20Kaura
Written for December 2014 by
Graham Buirski, MBBS, MRCP(UK), FRCR, FRANZCR, MD
Section Head MusculoSkeletal Imaging,
Sidra Medical and Research Center
Assistant Professor (Interim) of Clinical Radiology
Weill Cornell Medicine